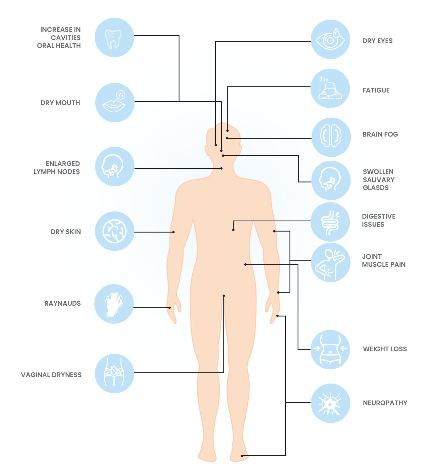
Sjögren's diagnosis complexities
Diagnosing Sjögren's disease often takes many years, as symptoms typically appear long before the condition is identified. The delay may be due to a lack of clinical awareness and the difficulty of problem solving the constellation of symptoms, even though Sjögren's disease is relatively common. As a result, many individuals with the condition remain undiagnosed. A Rheumatologist, Immunologist or Neurologist should be consulted as well as working in with a team of professionals including Ophthalmologists, Oral Medicine practitioners and Dentists.
Sjögren's disease tests
Common diagnostic tests for Sjögren's disease include eye exams such as a Schirmer's test where a result of equal to or less than 5mm of tears in 5 minutes may be indicative of autoimmune disease. Blood tests may also be used to look for common antibodies in Sjögren's (although not everyone will have these). Dentists may also be able to inspect the mouth for unusual dryness or inflammation. The gold standard for diagnosis is the finding of focal sialadenitis on a salivary gland biopsy.
A lip (salivary gland) biopsy may not be required in patients possessing serum positive SSA/anti-Ro antibodies (along with measured dry eye and mouth). Negative blood test results do not necessarily rule out the disease. Around 30-40% of people with Sjögren's disease are "seronegative", meaning they do not test positive for common autoantibodies like SSA/anti Ro and or SSB/Anti La . For many individuals, self-advocacy tools are helpful in collaborating with healthcare providers to achieve an accurate diagnosis.