
More info
Sjogrens disease commonly affects Women although that does not exclude Men as they can also be diagnosed as well.
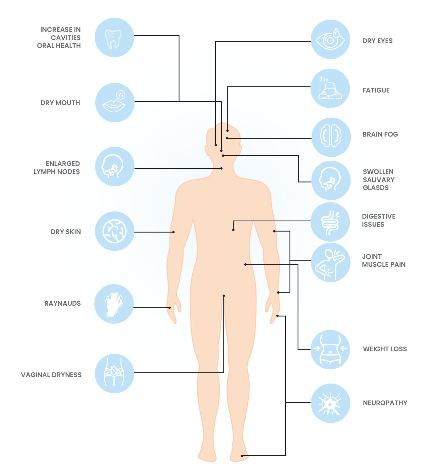
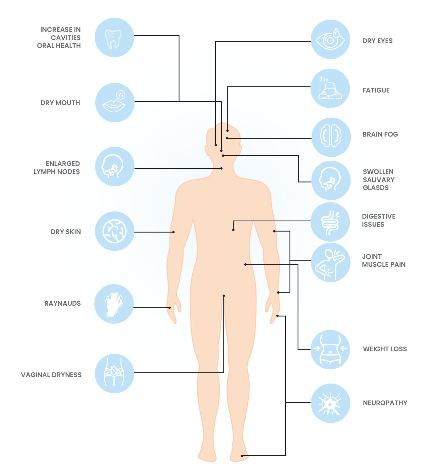
Sjögren's disease ("SHOW-grins") is a chronic systemic autoimmune disease where the immune system mistakenly attacks moisture-producing glands and other parts of the body.
Sjögren's disease can have a significant impact on the quality of life.
.
Diagnosis
Sjögren's disease commonly affects women, although men can be diagnosed as well. The disease can be overlooked during a diagnosis process; therefore, it is essential for patients to speak up and advocate for themselves if they feel something is wrong but are being dismissed. People who don't fulfil classification criteria but have features suspicious for Sjögrens such as low blood cells, high gamma globulin levels, inflamed lungs and muscles and neuropathies should be monitored closely.
Comorbidities
Patients often experience a range of comorbidities and understanding these conditions could help to improve the quality of life for those living with Sjögren’s disease. A multidisciplinary approach potentially involving Rheumatologists, Immunologists, Dentists, Opthamologists and mental health professionals is vital for managing comorbidities associated with Sjögren’s disease. Awareness and proactive management can significantly enhance patient outcomes and quality of life.
Causes
Sjögren’s disease is an autoimmune condition where the body’s immune system mistakenly attacks healthy tissues. In a typical immune response, the system defends the body against infections and disease. However, in Sjögren’s disease, the immune system targets the moisture-producing glands, particularly those responsible for tears and saliva, leading to inflammation and damage.
It is not currently fully understood why Sjögren's disease occurs. It is hypothesised that it may be a mix of genetic and environmental factors that may contribute to the development.
Sjögren's disease ("SHOW-grins") is a chronic systemic autoimmune disease where the immune system mistakenly attacks moisture-producing glands and other parts of the body.
Sjögren's disease can have a significant impact on the quality of life.
Diagnosis
Sjögren's disease commonly affects women, although men can be diagnosed as well. The disease is often overlooked in the diagnosis progress, so it is essential for patients to speak up and advocate for themselves if they feel something is wrong but are being dismissed. People who don't fulfil classification criteria but have features suspicious for Sjögrens such as low blood cells, high gamma globulin levels, inflamed lungs and muscles and neuropathies should be monitored closely.
Comorbidities
Patients often experience a range of comorbidities and understanding these conditions could help to improve the quality of life for those living with Sjögren’s disease. A multidisciplinary approach potentially involving rheumatologists, immunologists, dentists, opthamology and mental health professionals is vital for managing comorbidities associated with Sjögren’s disease. Awareness and proactive management can significantly enhance patient outcomes and quality of life.
Causes
Sjögren’s disease is an autoimmune condition where the body’s immune system mistakenly attacks healthy tissues. In a typical immune response, the system defends the body against infections and disease. However, in Sjögren’s disease, the immune system targets the moisture-producing glands, particularly those responsible for tears and saliva, leading to inflammation and damage.
It is not currently fully understood why Sjogrens disease occurs. It is hypothesised that it may be a mix of genetic and environmental factors that may contribute to its development.
.
List of services
-
Associated AutoimmuneItem link List Item 1
Sjögren’s disease frequently coexists with other autoimmune diseases, particularly rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE). These conditions share similar immune system dysfunctions, leading to joint pain, fatigue, and systemic inflammation. In these cases it may be labelled "associated" Sjögren's.
-
Raynaud’s PhenomenonItem link List Item 2
A common comorbidity, Raynaud’s phenomenon, is characterised by reduced blood flow to extremities such as fingers and toes, causing them to turn white or blue in response to cold or stress.
-
Thyroid DisordersItem link List Item 3
Autoimmune thyroid diseases, (including Hashimoto’s thyroiditis and Graves' disease) are more prevalent in Sjögren’s patients. These conditions affect metabolism, energy levels, and overall wellbeing.
-
LymphomaItem link List Item 4
Patients with Sjögren’s disease have an increased risk of developing non-Hodgkin's lymphoma. Regular monitoring and early detection are crucial for better outcomes. Studies show that men are at a higher risk.
-
Gastrointestinal DisordersItem Link
Many individuals with Sjögren’s experience gastrointestinal issues such as irritable bowel syndrome (IBS), acid reflux, and gastroparesis, impacting digestion and comfort.
-
NeurologicalItem Link
Neurological issues, including peripheral neuropathy (nerve pain, burning and tingling) and cognitive dysfunction often referred to as 'brain fog,' are common among Sjögren’s patients.
-
Mental HealthItem Link
Living with a chronic illness like Sjögren’s can lead to mental health challenges, including anxiety and depression, underscoring the importance of psychological support as part of holistic care.
-
Joint painItem Link
Sjögren's patients often report joint pain. This may be anywhere in the body but it is a common symptom. It is similar but not exactly the same as Rheumatoid arthritis.
-
FatigueItem Link
Fatigue is a common symptom, and it can be debilitating for many people with the condition. Around 70% of patients with primary Sjögren's disease experience disabling fatigue, which can significantly impact their quality of life.
Diagnosis complexities
Diagnosing Sjögren's disease often takes many years, as symptoms typically appear long before the condition is identified. The delay may be due to a lack of clinical awareness and the difficulty of problem solving the constellation of symptoms, even though Sjögren's disease is relatively common. As a result, many individuals with the condition remain undiagnosed. A Rheumatologist, Immunologist or Neurologist should be consulted as well as working in with a team of professionals including Ophthalmologists, Oral Medicine practitioners and Dentists.
Tests
Common diagnostic tests include eye exams such as a Schirmer's test where a result of equal to or less than 5mm of tears in 5 minutes may be indicative of autoimmune disease. Blood tests may also be used to look for common antibodies in Sjögren's (although not everyone will have these). Dentists may also be able to inspect the mouth for unusual dryness or inflammation. The gold standard for diagnosis is the finding of focal sialadenitis on a salivary gland biopsy.
A lip (salivary gland) biopsy may not be required in patients possessing serum positive SSA/anti-Ro antibodies (along with measured dry eye and mouth). Negative blood test results do not necessarily rule out the disease. Around 30-40% of people with Sjögren's disease are "seronegative", meaning they do not test positive for common autoantibodies like SSA/anti Ro and or SSB/Anti La . For many individuals, self-advocacy tools are helpful in collaborating with healthcare providers to achieve an accurate diagnosis.

Summary
Sjögren’s disease is an autoimmune condition where the body’s immune system mistakenly attacks healthy tissues. In a typical immune response, the system defends the body against infections and disease. However, in Sjögren’s disease, the immune system targets the moisture-producing glands, particularly those responsible for tears and saliva, leading to inflammation and damage. 9 in 10 patients are female and currently, there is no single determined cause of the disease.
Diagnosis
Sjögren's disease commonly affects women, although men can be diagnosed as well. The disease can be overlooked during a diagnosis process; therefore, it is essential for patients to speak up and advocate for themselves if they feel something is wrong but are being dismissed. People who don't fulfil classification criteria but have features suspicious for Sjögrens such as low blood cells, high gamma globulin levels, inflamed lungs and muscles and neuropathies should be monitored closely. Visit the diagnosis page for more information.
Comorbidities
Patients often experience a range of comorbidities and understanding these associated conditions could help to improve the quality of life for those living with Sjögren’s disease. See below for more information.
Exclusions in testing
Sjögren's disease overlaps with many other medical problems such as allergies, therefore these must be excluded throughout the diagnostic process.
The vast majority of people with dry eye and dry mouth do not have an autoimmune disease, therefore positive autoantibodies or biopsy can help confirm or exclude positive autoimmunity and false negatives can occur, particularly in children and young adults. People who don't fulfil classification criteria but have features suspicious for Sjögren's such as low blood cells, high gamma globulin levels, inflamed lungs and muscles and neuropathies should be monitored closely.
Please see the Treatment for Sjögren's page to dive further into the details of the diagnostic tests
*Stats supplied by The Sjögren's Foundation USA
Origin
The disease is named after Dr. Henrik Sjögren, a Swedish ophthalmologist who first described the condition in the 1930s after observing a group of women with arthritis and severe dryness of the eyes and mouth.
To learn more about Sjogren's Disease causes, symptoms, diagnosis, and treatment, click the button below to view the full Wikipedia article.
Diagnosis complexities
Diagnosing Sjögren's disease often takes many years, as symptoms typically appear long before the condition is identified. The delay may be due to a lack of clinical awareness and the difficulty of problem solving the constellation of symptoms, even though Sjögren's disease is relatively common. As a result, many individuals with the condition remain undiagnosed.
A Rheumatologist, Immunologist or Neurologist should be consulted as well as working in with a team of professionals including Ophthalmologists, oral medicine practitioners and Dentists.
Associated illness
Sjögren’s disease frequently coexists with other autoimmune diseases, particularly rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE). These conditions share similar immune system dysfunctions, leading to joint pain, fatigue, and systemic inflammation. In these cases it may be labelled "associated" Sjögren's.
A common comorbidity, Raynaud’s phenomenon, is characterised by reduced blood flow to extremities such as fingers and toes, causing them to turn white or blue in response to cold or stress.
Autoimmune thyroid diseases, including Hashimoto’s thyroiditis and Graves' disease are more prevalent in Sjögren’s patients. These conditions affect metabolism, energy levels, and overall wellbeing.
Patients with Sjögren’s have an increased risk of developing non-Hodgkin's lymphoma. Regular monitoring and early detection are crucial for better outcomes. Studies show that men are at a higher risk.
Many individuals with Sjögren’s experience gastrointestinal issues such as irritable bowel syndrome (IBS), acid reflux, and gastroparesis, impacting digestion and comfort.
Neurological issues, including peripheral neuropathy (nerve pain, burning and tingling) and cognitive dysfunction often referred to as 'brain fog,' are common among Sjögren’s patients.
Living with a chronic illness like Sjögren’s can lead to mental health challenges, including anxiety and depression, underscoring the importance of psychological support as part of holistic care.
Sjögren's patients often report joint pain. This may be anywhere in the body but it is a common symptom. It is similar but not exactly the same as rhematoid arthritis.
Fatigue is a common symptom, and it can be debilitating for many people with the condition. Around 70% of patients with primary Sjögren's (pSS) experience disabling fatigue, which can significantly impact their quality of life.
Testing
Common tests
Common diagnostic tests include eye exams such as a Schirmers test where a result of equal to or less than 5mm of tears in 5 minutes may be indicative of autoimmune disease. Blood tests may also be used to look for common antibodies in Sjögren's (although not everyone will have these) Dentists may also be able to inspect the mouth for unusual dryness or inflammation. The gold standard for diagnosis is the finding of focal sialadenitis on a salivary gland biopsy.
Exlusions
Sjögren's disease overlaps with many other medical problems such as allergies, therefore these must be excluded throughout the diagnostic process.
The vast majority of people with dry eye and dry mouth do not have an autoimmune disease, therefore positive autoantibodies or biopsy can help confirm or exclude positive autoimmunity and false negatives can occur, particularly in children and young adults. People who don't fulfil classification criteria but have features suspicious for Sjögren's such as low blood cells, high gamma globulin levels, inflamed lungs and muscles and neuropathies should be monitored closely.
Please see the Diagnosis page for Sjögren's page to dive further into the details of the diagnostic tests.
*Stats supplied by The Sjögren's Foundation USA
